Canavan Disease
Contents
Summary
For the disease that we have assigned to you, look up the diesease in Wikipedia, OMIM, HGMD and any other resource you find. Document the resources you have found in this Wiki (resources section). Produce a 5 min presentation for our first practical session.
Names
NAMES * named after Myrtelle Canavan, the experts who first described the disorder in 1931. * aspartoacylase deficiency * aminoacylase 2 deficiency * Canavan-Van Bogaert Bertrand disease * SPONGY DEGENERATION OF CENTRAL NERVOUS SYSTEM ASPARTOACYLASE DEFICIENCY * ASPA DEFICIENCY * ASP DEFICIENCY * ACY2 DEFICIENCY
Inheritance
INHERITANCE * autosomal recessive * Each pregnancy of a couple, both heterozygous, for a disease-causing mutation in ASPA has a 25% chance of resulting in a child with Canavan disease, a 50% chance of being an asymptomatic carrier, and a 25% chance of being unaffected and not a carrier. * often in persons of Ashkenazi (German and Eastern European) Jewish ancestry. It is estimated that 1 in 40 Ashkenazi Jews is a carrier of the Canavan gene. It is also found in other ethnic groups. In fact, thanks to the success of ongoing screening programs in the Jewish population, most of the children born with Canavan disease today have no known Jewish heritage. * Ashkenazi Jews from Lithuania, eastern Poland, and Russia, and amongst the Saudi Arabians.
Diagnosis
DIAGNOSIS PRENATAL * due to screening programs. * Canavan disease is inherited in an autosomal recessive manner. Each pregnancy of a couple in which both partners are heterozygous for a disease-causing mutation in ASPA has a 25% chance of resulting in a child with Canavan disease, * DNA testing tells you whether you are a carrier of the Canavan Disease * Carrier testing is available on a population basis for individuals of Ashkenazi Jewish heritage. Carrier testing for at-risk relatives and prenatal testing for pregnancies at increased risk are possible when the disease-causing mutations in the family are known. For couples in which one partner is known to be a carrier and the carrier status of the other is unknown, prenatal testing can be performed by measuring the concentration of NAA in amniotic fluid at 16 to 18 weeks’ gestation. * Molecular genetic testing. Prenatal testing for pregnancies at 25% risk is possible by analysis of DNA extracted from fetal cells obtained by chorionic villus sampling (CVS) at approximately ten to 12 weeks' gestation or by amniocentesis usually performed at approximately 15 to 18 weeks' gestation. Both disease- causing alleles present in the family must be identified before prenatal testing can be performed. Note: Gestational age is expressed as menstrual weeks calculated either from the first day of the last normal menstrual period or by ultrasound measurements. * Biochemical genetic testing. For couples in which one partner is known to be a carrier and the mutation or carrier status of the other is unknown, prenatal testing can be performed by measuring the level of NAA in amniotic fluid at 15 to 18 weeks’ gestation [Bennett et al 1993, Al-Dirbashi et al 2009]. *Preimplantation genetic diagnosis (PGD) may be available for families in which the disease-causing mutations have been identified [Yaron et al 2005]. For laboratories offering PGD, see. Note: It is the policy of GeneReviews to include clinical uses of testing available from laboratories listed in the GeneTests Laboratory Directory; inclusion does not necessarily reflect the endorsement of such uses by the author(s), editor(s), or reviewer(s). POSTNATAL * Increased N-acetyl-L-aspartic acid (NAA) in urine, CSF, and blood. * Symptoms usually become apparent when the infant is three to nine months old. * Neuroimaging * Reduced aspartoacylase activity in cultured skin fibroblasts * Spongy degeneration of brain on histology * deficiency of the enzyme aspartoacylase in skin cells or by testing the gene for Canavan disease in the blood. MILD / JUVENILE * In mild/juvenile Canavan disease NAA may only be slightly elevated; thus, the diagnosis relies on molecular genetic testing of ASPA, the gene encoding the enzyme aspartoacylase. Such testing is available on a clinical basis. * In individuals with mild/juvenile Canavan disease, neuroimaging may not be helpful. * Mild/juvenile Canavan disease is characterized by mild developmental delay that can go unrecognized. Head circumference may be normal.
Testing
TESTING. N-Acetylaspartic acid (NAA) Urine: The concentration of NAA in the urine can be measured using gas chromatography-mass spectrometry (GC-MS) [Michals & Matalon 2011]. Control values in one series (n=48) were 23.5±16.1 μmol/mmol creatinine. In neonatal/infantile (severe) Canavan disease the mean concentration of NAA (n=117) was 1440.5±873.3 μmol/mmol creatinine. In mild/juvenile Canavan disease, mild elevation of NAA may be found, (n=2) 106 μmol/mmol creatine Amniotic fluid: The concentration of NAA can be measured in the amniotic fluid by stable-isotope dilution and GC-MS or by liquid chromatography tandem mass spectrometry [Bennett et al 1993, Al Dirbashi et al 2009]. NAA concentration in amniotic fluid was 0.30-2.55 μmol/L in controls and 8.68 μmol/L in an affected pregnancy [Bennett et al 1993]. Aspartoacylase enzyme activity Skin fibroblasts Although aspartoacylase enzyme activity can be assayed in cultured skin fibroblasts, it may not be reliable because the activity varies with culture conditions. Individuals with severe Canavan disease often have unmeasurable enzyme activity. Carriers of alleles associated with severe Canavan disease have about one-half normal enzyme activity [Matalon et al 1993]. White blood cells and thrombocytes. Aspartoacylase enzyme activity is not detectable in white blood cells or platelets. Amniocytes/CVS Aspartoacylase enzyme activity is extremely low in normal amniocytes and chorionic villus sampling (CVS). Enzyme activity cannot be relied upon for prenatal testing [Bennett et al 1993]. Clinical testing: Targeted mutation analysis (A) Two mutations, p.Glu285Ala and p.Tyr231X, account for 98% of disease-causing alleles in the Ashkenazi Jewish population and 3% of alleles in non-Ashkenazi Jewish populations [Michals & Matalon 2011]. One mutation, p.Ala305Glu, accounts for 30%-60% of disease-causing alleles in non-Ashkenazi Jewish populations and approximately 1% of alleles in the Ashkenazi Jewish populations [Kaul et al 1994b, Elpeleg & Shaag 1999]. Sequence analysis (B) of the ASPA coding region is available for individuals in whom mutations were notidentified by targeted mutation analysis. Note: (1) The c.433-2A>G splice site mutation found in a single Ashkenazi Jewish family should not be considered a typical Ashkenazi Jewish mutation. (2) More than 50 other mutations have been reported in non- Ashkenazi Jewish populations [Kaul et al 1994b, Elpeleg & Shaag 1999, Olsen et al 2002, Zeng et al 2002, Michals & Matalon 2011]. Deletion/duplication analysis. (C) Deletions and duplications are not detectable by sequence analysis; other methods need to be used. Deleted segments of various sizes of cDNA have been reported [Zeng et al 2006, Kaya et al 2008].The authors encountered two individuals with complete deletion of ASPA and two with partial deletions [Matalon, unpublished data].
Method Mutations Detected Mutation Mutation
Frequency in Frequency in NON
(A) p.Glu285Ala, p.Tyr231X 98 3
p.Ala305Glu 1 30-60
(B) Sequence variants N/A 87 (C) Large, comprising one or more exons N/A (<10)
Note: Although NAA concentration is also elevated in the blood and CSF of children with neonatal/infantile (severe) Canavan disease, the number of affected individuals evaluated to date is small [Michals & Matalon 2011].
Treatment
HOW DOES THE TREATMENT IMPROVE PHENOTYPE? CURE * At the present time there is no cure for Canavan disease. TREATMENT NOTE * treatment for Canavan disease is supportive and depends on symptom management. * the Canavan disease treatment is supportive and symptomatic. * Neonatal/infantile Canavan disease: Treatment is supportive and directed to providing adequate nutrition and hydration, managing infectious diseases, and protecting the airway. Physical therapy minimizes contractures and maximizes motor abilities and seating posture; special education programs enhance communication skills. Seizures are treated with antiepileptic drugs. Gastrostomy may be needed to maintain adequate food intake and hydration when swallowing difficulties exist. PRENATAL * Several laboratories proffer pre- natal screening for the disease to populations that are at risk. Researchers have devised animal models and are using them to assess possible treatment strategies. Studies to comprehend how the brain normally develops and functions and how it gets affected by genetic mutation are carried out. These studies help better understand Canavan disease; and thus offer greater likelihood to new possibilities of treatment. NEONATAL / INFANTILE * Treatment is supportive and directed to providing adequate nutrition and hydration, managing infectious diseases, and protecting the airway. * Children benefit from physical therapy to minimize contractures and to maximize abilities and seating posture, from other therapies to enhance communication skills (especially in those with a more gradual clinical course), and from early intervention and special education programs. * Seizures may be treated with antiepileptic drugs (AEDs). * A feeding gastrostomy may be required to maintain adequate intake and hydration in the presence of swallowing difficulties. * Diamox® seems to reduce intracranial pressure. * Botox® injections may be used to relieve spasticity. * Convulsions and seizures are handled suitably using anti-convulsants. JUVENILE / MILD * These individuals may require speech therapy or tutoring but require no special medical care. FUTURE WORK HUMAN * Furthermore, there are investigational clinical trials of gene therapy. In the study a normal gene is cloned to work instead of the faulty one that is known to result in Canavan disease. * Gene transfer to the brains of two children with Canavan disease using a nonviral vector was well tolerated [Leone et al 2000, Janson et al 2002]. Some biochemical, radiologic, and clinical changes may have occurred; however, the children continued to follow the course of those with untreated Canavan disease. * In ten children with Canavan disease, multisite injection with AAV2 as the vector for ASPA was well tolerated [McPhee et al 2006]. Three developed AAV2 neutralizing antibodies. No children improved. * Lithium citrate may reduce N-acetylaspartic acid (NAA) concentration in the brain. Six persons with Canavan disease given lithium citrate for 60 days were reported to have reduced NAA in the basal ganglia and mild improvement in frontal white matter [Assadi et al 2010]. The clinical significance of use of lithium citrate is not known. * The enzyme defect in Canavan disease leads to decreased levels of acetate in the brain. In a clinical trial with glycerol triacetate in two persons with Canavan disease the compound was well tolerated; however, there was no clinical improvement [Madhavarao et al 2009]. It is speculated that higher doses of glycerol triacetate may be needed. * There is an investigational therapy using lithium citrate. A person diagnosed with Canavan Disease demonstrated elevated levels of N-acetyl aspartate. Lithium citrate has been used for experimentation in a rat genetic model of Canavan Disease; and results showed it appreciably reduced levels of N-acetyl aspartate. When the dug was administered to a human, the patinet reversed during the 2 week wash-out period, after the removal of lithium. Evidence suggests that a larger controlled clinical study and research of lithium is necessary to use it as supportive therapy for children having Canavan disease. and lithium citrate, used in a rat model of Canavan Disease showed that levels of N-acetyl aspartate were greatly decreased. A larger clinical study and research of lithium is essential to manage children diagnosed with Canavan disease. ANIMAL * A knock-out mouse has been created, with a phenotype similar to that of human Canavan disease [Matalon et al 2000]. This model is being used to investigate pathophysiology [Surendran et al 2004] gene therapy and other modes of treatment [Matalon et al 2003]. * Gene therapy with AAV2 was given to knock-out Canavan disease mice: localized improvement did not spread to the entire brain [Matalon et al 2003]. * Stem cell therapy in knock-out Canavan disease mice was done in collaboration with Genzyme Corporation: The stem cells produced some oligodendrocytes but not enough to make myelin [Surendran et al 2004]. * Enzyme replacement therapy using native ASPA and pegylated ASPA (i.e., ASPA in which covalent attachment of polyethylene glycol polymer chains masks the enzyme from the host allowing for longer circulation and less renal clearance) were injected into the peritoneum of Canavan disease mice. Preliminary results show that the enzyme passed the blood brain barrier and there was a decrease of NAA in the brain. These experiments were short term; longitudinal studies are being planned [Zano et al 2011]. * A mouse that seems to have a Canavan disease phenotype was produced by using the mutagen ethylenenitrosourea (ENU) to change the residue Gln193 to a termination codon in exon 4 (577C>T) [Traka et al 2008].
Phenotype
Phenotypic description of the disease.
(Describe this in your own words, avoid plagiarism. Summarise the information from different sources.)
PHENOTYPIC DESCRIPTION OF THE DISEASE. HEAD * incresing head circumference * lack of head control * Over time they may become developmentally delayed * Mental impairment * Megalocephaly / Macrocephaly or a big head * Mental retardation and mental impairment EYE * reduced visual responsiveness * Over time they may become blind and have trouble swallowing * Blindness * Optic Atrophy * Nystagmus EAR * Deafness, loss of hearing SPEECH * children with canavan disease cannot talk. * Difficulties in feeding * the children are very quiet, BODY, MUSCLES * Over time they may suffer seizures, become paralyzed, * Seizures * paralysis * lacking energy, sluggish and indifferent. * convulsions and seizures * listless, lethargic and indifferent * Hypotonia eventually changes to spasticity. * abnormal muscle tone - stiffness / floppyness * Children with Canavan disease cannot crawl, walk, sit * Poor muscle tone, i.e., droopiness / limpness, or extreme stiffness and rigidity * Loss of formerly attained motor skills * The patient shows droopiness and limpness or rigidity and stiffness of the body NEUROLOGICAL * Demyelination with white matter disease in internal capsule, external capsule, genu of corpus callosum, subcortical white matter, and posterior fossa Brain atrophy LIFE * death within first decade (some up two first decades) * Mild/juvenile Canavan disease is characterized by mild developmental delay that can go unrecognized. Head circumference may be normal.
Cross-references
See also description of this disease in
- specific link to Wikipedia
- specific link to HGMD
- specific link to OMIM
... (see databases in "resources")
Biochemical disease mechanism
The example protein is involved in the example pathway...
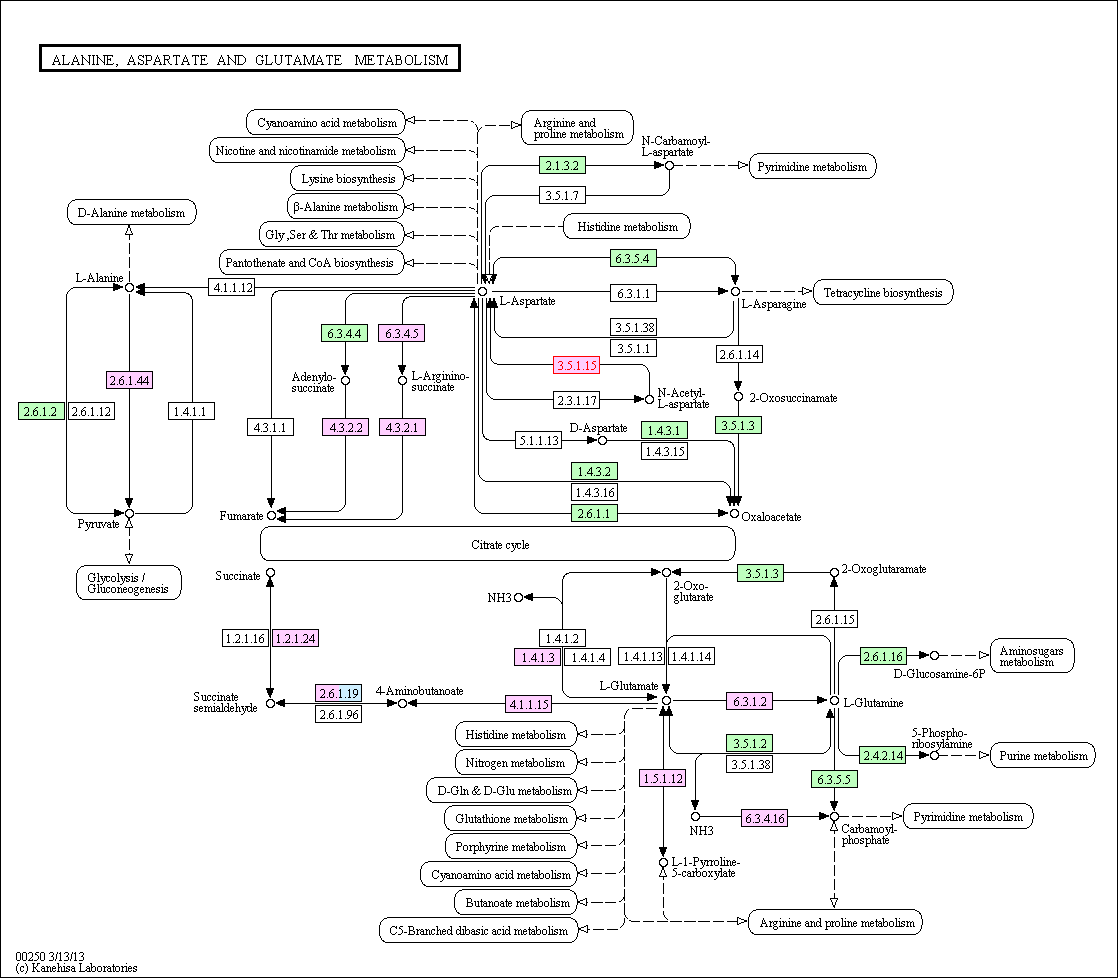
* KEGG
* belongs to a group of inherited diseases called the leuko-dystrophies.
These disorders cause defective development of the myelin sheath, (the casing that functions like an insulator / a protective cover for the nerves and also conducts nerve impulses) in the brain. Myelin is a substance that comprises of 10 special chemicals. Each category or type of leukodystrophy has an impact on only one of these chemicals.
* Canavan disease causes defective development of the myelin sheath that covers the nerve fibers. The primary cause for the disorder is a defective / malfunctioning ASPA gene. The ASPA gene is in charge for the synthesis of enzyme aspartoacyclase. Aspartoacyclase decomposes the brain molecule N acetyl aspartate. Thus, impaired functioning of the aspartoacylase does not allow normal decomposition of N-acetyl aspartate, and as a result, a lack of break-down hampers the normal synthesis and the development of myelin.
* the white matter of the brain degenerates in to soft tissue and has tiny fluid filled spaces
* One of the chief Canavan Disease causes is a malfunctioning / faulty ASPA gene. This gene is in charge of the synthesis of the enzyme aspartoacyclase. This enzyme breaks down the concentrated brain molecule N acetyl aspartate. Reduced activity and functioning of the aspartoacylase puts a stop to the normal decomposition of N-acetyl aspartate, and consequently, a lack of break down hinders the normal production and the development of the myelin sheath of the nerves.
* The components of N-acetylaspartate acid (NAA) are involved in forming the myelin sheathe. Normally, aspartoacyclase, decomposes NAA in to the units that are required. However, in Canavan Disease, mutation affects the manufacture of this enzyme (experts say this is the primary Canavan disease cause). NAA build up to unsafe levels, obstructing the brain's transmission network.
Ideally, include a graphical pathway representation like this one:
(see above: own words, no plagiarism)
Cross-references
- link to KEGG
- link to MetaCyc
... see databases in "resources"
Mutations
Current knowledge about mutations associated with the disease. - Separate into disease causing and neutral mutations. -- These sequence pages will be the starting point for collecting prediction results and result discussions.
Note: Until further notice you only need to care about the reference sequence pages. -- At a later stage we will assign mutations we expect you to work on. Then, it will make sense to create on page per mutation that is assigned to you.
GENE
* The gene that is linked to the disease is situated on chromosome 17.
* 17p13.2
* ASPA - ASPARTOACYLASE
* Normal allelic variants. The gene comprises 29 kb with six exons and five introns. The exons vary in size from 94 bp (exon 3) to 514 bp (exon 6).
* Pathologic allelic variants. See Table 2. The major disease-causing allelic variants are p.Glu285Ala, p.Tyr231X, and p.Ala305Glu. (For more information, see Table A.)
* Normal gene product. Aspartoacylase is a protein of 313 amino acids, suggesting a molecular weight of 36 kd [Kaul et al 1993]. The 93% homology of the amino acid and nucleotide sequence of human and bovine aspartoacylase suggest a high degree of conservation of this enzyme in mammals [Kaul et al 1994a]. The protein is observed in most tissues. Recent studies have shown that ASPA is a dimer with zinc at the catalytic site analogous to other carboxypeptidases. Mutations caused conformational changes that affect the activity of the enzyme [Bitto et al 2007].
* Abnormal gene product. Aspartoacylase is responsible for hydrolyzing N-acetylaspartic acid (NAA) into aspartic acid and acetate. The abnormal alleles include null mutations, which make no aspartoacylase, and missense mutations, which make less active forms of aspartoacylase. Although aspartoacylase is expressed widely throughout the body, its absence in the CNS leads to the specific build-up of NAA in the brain that causes demyelinization and other signs of the disease.
Gene Symbol Chromosomal Locus Protein name Locus specific HGMD ASPA 17p13.2 Aspartoacylase ASPA @ LOVD ASPA
DNA Nucleotide Change Protein Amino Acid Change c.433-2A>G -- c.693C>A p.Tyr231X c.854A>C p.Glu285Ala c.863A>G p.Tyr288Cys c.914C>A p.Ala305Glu
Reference sequence
Which sequence does not cause the disease and is most often found in the population.