Difference between revisions of "Hemochromatosis 2012"
(→Disease causing mutations) |
(→Reference sequence) |
||
| Line 82: | Line 82: | ||
MGPRA<font color="red">R</font>PALLLLMLLQTAVLQGRLLRSHSLHYLFMGASEQDLGLSLFEALGY<font color="red">V</font>DDQLF<font color="red">V</font>F |
MGPRA<font color="red">R</font>PALLLLMLLQTAVLQGRLLRSHSLHYLFMGASEQDLGLSLFEALGY<font color="red">V</font>DDQLF<font color="red">V</font>F |
||
| − | YD<font color="red">H</font>E<font color="red"> |
+ | YD<font color="red">H</font>E<font color="red">S</font>RRVEP<font color="red">R</font>TPWVSSRISSQMWLQLSQSLK<font color="red">G</font>WDHMFTVDFWT<font color="red">I</font>MENHNHSKESHTLQV |
ILGCEM<font color="red">Q</font>EDNSTEGYWKYGYDGQDHLEFCPDTLDWRAAEPRAWPTKL<font color="red">EW</font>ERHKIR<font color="red">A</font>RQNR |
ILGCEM<font color="red">Q</font>EDNSTEGYWKYGYDGQDHLEFCPDTLDWRAAEPRAWPTKL<font color="red">EW</font>ERHKIR<font color="red">A</font>RQNR |
||
AY<font color="red">L</font>ERDCPAQLQQLLELGRGVLDQQVPPLVKVTHHVTSSVTTL<font color="red">R</font>CRALNYYPQNITMKWL |
AY<font color="red">L</font>ERDCPAQLQQLLELGRGVLDQQVPPLVKVTHHVTSSVTTL<font color="red">R</font>CRALNYYPQNITMKWL |
||
| − | KDKQPMDAKEFEPKDVLPNGDGTYQGWITLA<font color="red">V</font> |
+ | KDKQPMDAKEFEPKDVLPNGDGTYQGWITLA<font color="red">V</font>PPGEEQRYT<font color="red">CQ</font>VEHPGLDQPLI<font color="red">V</font>IWEPS |
PSGTLVIGVISGIAVFVVILFIGILFIIL<font color="red">R</font>KRQGSRGAMGHYVLAERE |
PSGTLVIGVISGIAVFVVILFIGILFIIL<font color="red">R</font>KRQGSRGAMGHYVLAERE |
||
This protein has a length of 348 amino acids and the red positions indicate the positions of known mutations. |
This protein has a length of 348 amino acids and the red positions indicate the positions of known mutations. |
||
Revision as of 10:23, 22 April 2012
Under construction...
Contents
Summary
Hereditary hemochromatosis is an autosomal recessive monogenetic metabolic disease caused by mutations in the HFE gene. Malfunction of the HFE gene leads to an increased absorption of iron in the intestines. It was first described in a diabetes report by Armand Trousseau in 1865.
The high iron concentration within the body can cause several side-effects like arthritis, diabetes, heart muscle disorders, hepatic cirrhosis, hyperpigmentation, and hypopituitarism. Because the accumulation of iron is a slow process most patients show symptoms between the age of 30 to 60.
Though this site focuses on hereditary hemochromatosis (hemochromatosis type 1) it is worth noting, that there are differrent types of hemochromatosis.
- Hereditary hemochromatosis (type 1) - autosomal recessive; gene: HFE
- Juvenile hemochromatosis (type 2A and type 2B) - autosomal recessive; genes: HJV (2A) / HAMP (2B)
- Hemochromatosis type 3 - autosomal recessive; gene: TFR2
- Hemochromatosis type 4 - autosomal dominant; gene: SLC40A1
Cross-references
- Hemochromatosis type 1 (OMIM)
- Hemochromatosis type 2A (OMIM)
- Hemochromatosis type 2B (OMIM)
- Hemochromatosis type 3 (OMIM)
- Hemochromatosis type 4 (OMIM)
Prevalence
Hereditary hemochromatosis is quite common, especially in groups with european ancestry. It has a prevalence of about 2 to 3 in 1000 and a carrier rate of about 10 percent.
Phenotype
Hereditary hemochromatosis leads to an unregulated absorption of dietary iron. Due to the increased concentration of iron within the body, other dysfunctions can occur depending on the tissue.
- The accumulation of iron causes a brown coloring of the skin (hyperpigmentation). This can be seen especially well in the armpits, but also on internal organs like the liver.
- Iron deposits in the joints can lead to arthritis.
- A high concentration of iron in the pituitary gland decreases the secretion of hormones (hypopituitarism). This can cause further effects like testicle dysfunction and the loss of sex drive.
- In the liver it can lead to liver cirrhosis, in the heart to heart muscle disorders (cardiomyopathy).
- Iron also aids the creation of free radicals which can damage the DNA and cause cancer.
- In the blood iron competes with chromium for the binding to transferrin. Chromium is important for the normal function of insulin. This disturbance of chromium (due to too much iron) can lead to diabetes.
Men show these symptoms more often than women. This is due to the loss of blood (and iron) during menstruation and pregnancy. The rate of iron accumulation also depends on the diet of the patient. Most patients begin to show symptoms between the age of 30 and 60.
Cross-references
See also description of this disease in:
HFE Gene
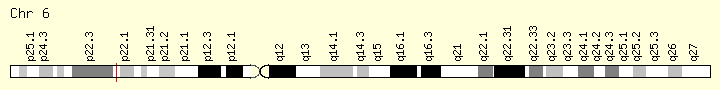
The HFE gene is located on the short arm of the sixth chromosome.
It has a length of 11,124 bases and lies on the plus strand. It further contains six exons, coding for the protein, with a length of 1047 bases.
HFE protein
The protein coded by the HFE gene consists of 4 chains, with 2 different entities in total, the HFE chain and the Beta-2-Microglobulin chain.
HFE chain
The HFE chain of the protein consists of 8 helices, encoded by 70 residues, and 20 strands, coded by 109 residues.
Beta-2-Microglobulin
The Beta-2-Microglobulin chain consists of 11 strands, which are encoded by 51 residues.


Cross-references
Biochemical disease mechanism

Under normal circumstances, iron is absorpt in the intestines and bound to transferrin. This iron loaded transferrin then associates with the transferrin receptor (TFRC) for further transport through the body. HFE forms a complex with TFRC to reduce its affinity for iron-loaded transferrin and to partially inhibit the release of the iron once the complex reaches the target cells. Further it seems that HFE plays a role in a sensory pathway to determine the iron concentration within the body and to regulate the absorption of iron through the expression of DMT1 (divalent metal transporter).

The different mutations in the HFE gene diminish or inhibit these functions. C282Y affects the beta-2-microglobulin binding site and prevents the formation of the HFE-TFRC-complex. H63D does not prevent the formation of the complex, but reduces the inhibitory functions of HFE. This causes the increased iron uptake and accumulation of iron within the cells that is associted with hereditary hemochromatosis.
Dysfunctional HFE seems also to lead to a lack of hepcidin, another protein that (down-)regulates the iron uptake.
Cross-references
Mutations
Reference sequence
KEGG lists the occurring protein sequence as follows:
MGPRARPALLLLMLLQTAVLQGRLLRSHSLHYLFMGASEQDLGLSLFEALGYVDDQLFVF YDHESRRVEPRTPWVSSRISSQMWLQLSQSLKGWDHMFTVDFWTIMENHNHSKESHTLQV ILGCEMQEDNSTEGYWKYGYDGQDHLEFCPDTLDWRAAEPRAWPTKLEWERHKIRARQNR AYLERDCPAQLQQLLELGRGVLDQQVPPLVKVTHHVTSSVTTLRCRALNYYPQNITMKWL KDKQPMDAKEFEPKDVLPNGDGTYQGWITLAVPPGEEQRYTCQVEHPGLDQPLIVIWEPS PSGTLVIGVISGIAVFVVILFIGILFIILRKRQGSRGAMGHYVLAERE
This protein has a length of 348 amino acids and the red positions indicate the positions of known mutations.
Disease causing mutations
Arg-Ser 6 Val Met 53 Val-Met 59 His-His 63 His-Asp 63 Ser-Cys 65 Arg-Term 71 Gly-Arg 93 Ile-Thr 105 Gln-His 127 Glu-Gln 168 Glu-Term 168 Trp-Term 169 Ala-Val 176 Leu-Pro 183 Arg-Gln 224 Val-Leu 272 Cys-Tyr 282 Cys-Ser 282 Gln-Pro 283 Val-Ala 295 Arg-Met 330 the mutations are listed as fromAA-toAA atPosition#
Where C282D and H63D seem to be the most common.
Deletions
small
AGTCGC^67CGTGtGGAGCCCCGA AGTCTG^92AAAGgGTGGGATCAC ATTGG^156AGAGCaGCAGAACCCA GCAGCA^159GAACcCAGGGCCTGG
gross
22 bp cd 50 nt.370 (described at genomic DNA level) 32744 bp incl. entire gene [Alu mediated] (described at genomic DNA level)
Insertions
GGACC^264TACCAaGGGCTGGATA
Disease causing splicings
IVS2 ds +4 T-C IVS3 ds +1 G-T IVS5 ds +1 G-A
complex rearrangements
c.[128G>A;187C>G], p.[G43D;H63D]
Cross-references
Diagnosis
Diagnosis of hereditary hemochromatosis can be achieved by multiple methods.
- Blood test: Measurement of the transferrin saturation or the serum ferritin concentration in the blood. Values that are significantly above the normal levels can be an indicator for hemochromatosis.
- Liver biopsy: Extraction and examination of liver tissue. A high concentration of iron within the liver corresponds to a high concentration of iron in the body.
- MRI: Magnetic resonance imaging can also be used to determine the iron concentration within the liver.
If these methods show a risk for hemochromatosis, a genetic analysis for the known HFE mutations should be made.
Cross-references
Treatment
Hemochromatosis itself cannot be treated, but the symptoms can be prevented or lessened.
- Phlebotomy: Bloodletting can be used to decrease the iron concentration. At first, about 500ml of blood are extracted once a week until the iron concentration reaches normal levels. Afterwards the extractions are scheduled to once every two to three months.
- Drugs: If the patient can’t handle frequent blood loss, chelating agents can be used. They bind the iron in the blood and increase its excretion through feces and urine. Examples are deferoxamine, deferasirox, and deferiprone.
- Diet: A low consumption of iron rich food decreases the rate of iron accumulation and therefore the development of the symptoms. It is also helpful to prevent the consumption of vitamin C about two hours before or after meals, because vitamin C aids the absorption of iron. Alcohol should also be avoided.
All of these treatments have to be continued throughout the whole life to keep the iron concentration within normal levels.
Cross-references
References
External links: